The Whipple Procedure: A Definitive Guide by a Master Surgeon
If you or a loved one have been told you need a Whipple Procedure, you are likely facing a serious diagnosis and a wave of complex information. We understand that this can be an overwhelming and deeply uncertain time. The Whipple procedure, known medically as a pancreaticoduodenectomy, is one of the most complex and demanding operations in modern medicine. It is also, for many patients, a life-saving surgery that offers the greatest hope for a cure.
This comprehensive guide is designed to demystify the surgical procedure whipple. Our goal is to provide you with clear, authoritative, and compassionate answers to your most urgent questions, from “what is a whipple procedure?” to the details of recovery and long-term outcomes. The success of this operation is profoundly linked to the skill of the surgeon. Here, under the leadership of world-renowned expert Prof. Dr. Oguzhan Karatepe, we combine the highest level of surgical mastery with the supportive care you need to navigate this journey with confidence.
Contact & WhatsApp: +90 530 917 30 30
Meet Prof. Dr. Oguzhan Karatepe: Your Whipple Procedure Specialist
There is no substitute for experience when it comes to the Whipple procedure. This is not just a general surgery; it is a specialized operation that should only be performed by surgeons with extensive, specific training and a high volume of cases. We are proud to have Prof. Dr. Oguzhan Karatepe, a world-class pancreatic surgeon, leading our team.
With an esteemed career spanning over 25 years, Prof. Dr. Karatepe is recognized globally as one of the leading whipple procedure surgeons. He has dedicated his career to mastering this and other complex abdominal cancer surgeries. His authority in the field is backed by more than 100 prestigious national and international academic publications and advanced training at the world’s foremost medical institutions. He has performed hundreds of these demanding operations, giving him the judgment and technical precision that are critical for patient safety and successful outcomes.
Patients from the USA, UK, Canada, Australia, and worldwide seek out Prof. Dr. Karatepe for his expertise in performing the surgical whipple procedure. They trust in his meticulous approach and his ability to offer hope in the most challenging of circumstances. When you choose our center, you are choosing a surgeon whose life’s work is dedicated to mastering the very operation you need.
What Is a Whipple Procedure (Pancreaticoduodenectomy)?
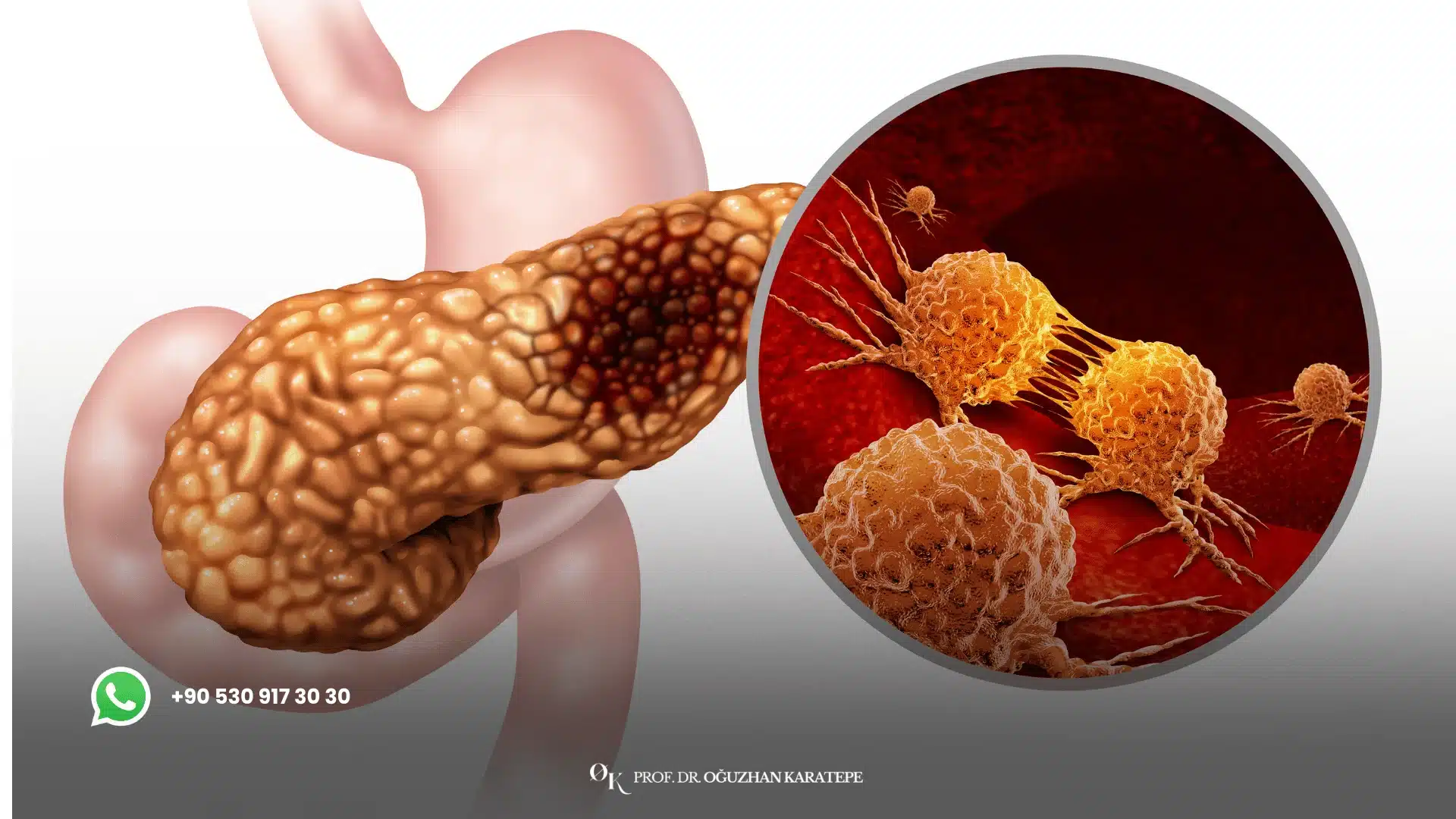
To fully answer “what is whipple procedure surgery?,” we must first understand its formal name: the pancreaticoduodenectomy whipple procedure. This name breaks down the core components of the operation. It is a major surgical intervention designed to remove tumors located in the “head” of the pancreas—the widest part of the organ, which is nestled in the curve of the small intestine.
The reason this operation is so extensive is due to the complex whipple procedure anatomy. The head of the pancreas shares a tightly woven network of blood vessels and ducts with several other vital organs. To ensure all of the cancerous tissue and surrounding lymph nodes are completely removed, the surgeon must remove not just the head of the pancreas, but also the adjoining organs. It is this extensive removal and the intricate reconstruction that follows that makes the Whipple procedure one of the most challenging operations for a surgeon to perform.
Contact & WhatsApp: +90 530 917 30 30

Why Is the Whipple Procedure Performed? Key Indications
The Whipple operation procedure is the standard and most effective treatment for a number of specific conditions affecting the head of the pancreas and surrounding structures.
Whipple Procedure for Pancreatic Cancer
The primary and most common reason for performing a Whipple’s procedure is for the treatment of pancreatic ductal adenocarcinoma located in the head of the pancreas. For patients with localized pancreatic cancer, the Whipple procedure offers the only potential chance for a cure. By removing the tumor and the nearby lymph nodes, the goal is to eliminate the cancer before it has a chance to spread.
Other Indications for the Whipple’s Procedure
While most commonly associated with pancreatic cancer and whipple procedure, this surgery may also be performed for:
- Cholangiocarcinoma: Cancer of the bile duct that is located near the pancreas.
- Duodenal Cancer: Cancer in the first part of the small intestine (the duodenum).
- Ampullary Cancer: Cancer that forms in the ampulla of Vater, where the bile duct and pancreatic duct join the small intestine.
- Benign Tumors or Cysts: Certain large, non-cancerous tumors or pre-cancerous cysts (like IPMNs) in the head of the pancreas that are causing symptoms or have a high risk of turning into cancer.
Contact & WhatsApp: +90 530 917 30 30
The Whipple Procedure Steps: A Detailed Walkthrough
Understanding the whipple procedure steps can help demystify this complex operation. The surgery is performed in two main phases: the resection (removal) phase and the reconstruction phase.
Phase 1: The Resection (What Is Removed)
During the first phase of the whipple surgery procedure, the surgeon meticulously dissects and removes all the diseased tissue. This includes:
- The Head of the Pancreas: The primary site of the tumor.
- The Duodenum: The C-shaped first portion of the small intestine, which is attached to the head of the pancreas.
- The Gallbladder: This organ is removed because it is attached to the bile duct.
- A Portion of the Bile Duct: The part of the bile duct that runs through the head of the pancreas is removed.
- Nearby Lymph Nodes: These are removed to check for any cancer spread and to help stage the disease accurately.
- A Portion of the Stomach (sometimes): In a classic Whipple, a small part of the stomach is removed. In a “pylorus-preserving” Whipple, the entire stomach and its valve (the pylorus) are preserved.
Phase 2: The Reconstruction (Putting It All Back Together)
After the removal is complete, the surgeon begins the highly intricate reconstruction phase. The goal is to re-establish the normal flow of the digestive system. This involves creating three new, carefully sutured connections (anastomoses):
- The Pancreas to the Intestine: The remaining body/tail of the pancreas is connected to the small intestine, allowing digestive enzymes to flow into the digestive tract.
- The Bile Duct to the Intestine: The remaining bile duct is connected to the small intestine, allowing bile from the liver to flow in and help with digestion.
- The Stomach to the Intestine: The stomach is connected to the small intestine, allowing food to pass from the stomach into the newly reconstructed digestive pathway.
This reconstruction is the most delicate part of the surgery whipple procedure and where the surgeon’s skill is most critical to prevent complications like leaks.
Contact & WhatsApp: +90 530 917 30 30
The Surgeon’s Role: Why Expertise Is Critical for the Whipple Procedure
When searching for whipple procedure surgeons, it is vital to understand that this is not a routine operation. The success, safety, and outcome of your surgery depend more on the surgeon’s experience than almost any other factor. Outcomes are consistently and significantly better at “high-volume” centers where surgeons perform this operation frequently.
An expert Whipple surgeon like Prof. Dr. Karatepe brings:
- Mastery of Complex Anatomy: The ability to safely work around critical blood vessels like the portal vein and superior mesenteric artery, which are in immediate contact with the pancreas.
- Technical Precision: The skill to create secure, leak-proof reconnections (anastomoses) with the soft, delicate pancreatic tissue.
- Sound Judgment: The experience to make critical decisions during the operation and to anticipate and manage potential challenges.
- Lower Complication Rates: High-volume surgeons have demonstrably lower rates of major complications and mortality.
Choosing an expert is the single most important step you can take to ensure the best possible outcome for your Whipple procedure pancreatic cancer treatment.
Contact & WhatsApp: +90 530 917 30 30
Whipple Procedure Recovery: What to Expect on Your Journey
The whipple procedure recovery is a marathon, not a sprint. It requires patience and a commitment to the recovery process.
- Hospital Stay: You can expect to be in the hospital for 1 to 2 weeks after surgery. During this time, your team will manage your pain, monitor for complications, and help you start moving. You may have several tubes and drains in place initially.
- Nutrition: You will start with IV fluids and slowly progress to clear liquids, and then to solid food over several days. Digestion will feel different, and you will need to eat small, frequent meals.
- At-Home Recovery: Full recovery takes time, often 2 to 3 months or more before you feel your energy levels return to near normal. You will have restrictions on lifting and driving for several weeks.
- Long-Term Adjustments: Life after a Whipple involves permanent dietary changes. You will likely need to take prescription pancreatic enzyme pills with every meal to help digest food properly. Your blood sugar will also be monitored closely.
Is the Whipple Procedure Worth It? A Candid Discussion
Patients and their families often ask, “is the whipple procedure worth it?“. This is a deeply personal and valid question given the magnitude of the surgery and the challenging recovery.
From a medical and curative standpoint, for a patient with a resectable pancreatic cancer, the answer is an overwhelming yes. The Whipple procedure is the only treatment that offers a chance of a cure and long-term survival. Without it, the cancer will inevitably progress.
The “worth” is measured against the alternative. While the recovery is difficult, it is a temporary challenge. The surgery provides the opportunity for more years of life—more time with family, more experiences, and more memories. It is a trade-off of a difficult few months for a chance at years of life. With a skilled surgeon and a supportive team, the journey is manageable, and the reward is invaluable.
Whipple Procedure Survival Rate: A Realistic Look at the Data
It is essential to have an honest discussion about the whipple procedure survival rate. The statistics can be intimidating, but they have improved dramatically over the last few decades. In the past, this was an operation with very high mortality. Today, at major centers of excellence, the mortality rate for the operation itself is less than 2-4%.
Regarding cancer survival, the rates depend on the stage of the cancer at the time of surgery. For patients who undergo a successful Whipple procedure for pancreatic cancer followed by chemotherapy, the 5-year survival rate can be as high as 20-30%. While this number may seem modest, it is a significant improvement and represents a real chance at a cure that does not exist without the surgery. Most importantly, these rates are highest when the surgery is performed by an expert surgeon who achieves a complete removal of the tumor (an R0 resection).
Contact & WhatsApp: +90 530 917 30 30
Key Takeaways
- A Complex, Life-Saving Surgery: The Whipple procedure is one of the most demanding operations, but it is the cornerstone of treatment for pancreatic head tumors.
- Expertise is Everything: Your outcome is directly tied to the experience of your surgeon. Choosing a high-volume, specialist Whipple procedure surgeon is critical.
- A Two-Phase Operation: The surgery involves a meticulous resection (removal) phase and an intricate reconstruction phase.
- Recovery is a Marathon: Be prepared for a lengthy but manageable recovery period. The goal is a return to a good quality of life.
- Hope is Real: The Whipple procedure survival rate has improved significantly, and this surgery offers the only potential cure for localized pancreatic cancer.

Your Next Step: A Consultation with a Whipple Expert
Being told you need a Whipple procedure is a profound moment that demands a clear and expert-led plan. The path forward can seem daunting, but the most important step you can take right now is to ensure you are in the hands of a true master of this operation. A consultation or a second opinion with a high-volume specialist can provide immense clarity, peace of mind, and the confidence that you are pursuing the best possible treatment path.
Prof. Dr. Oguzhan Karatepe has dedicated his life’s work to performing this exact surgical procedure whipple. His over 25 years of experience are your greatest asset. He has guided hundreds of patients and their families through this journey, combining his world-class technical skill with the deep compassion and support that this diagnosis requires. We understand the physical and emotional challenges you are facing, and we are here to meet them with an unparalleled level of expertise.
For an operation this important, you deserve nothing less than one of the world’s leading surgeons. We are here to provide that for you.
Contact us now to arrange a confidential consultation for yourself or your loved one. An expert opinion is the first step toward a successful outcome. Let us help you navigate this path with confidence and hope.
Contact & WhatsApp: +90 530 917 30 30
Frequently Asked Questions (FAQ) About the Whipple Procedure
Basics of the Whipple Procedure
1. What is a Whipple procedure?
The Whipple procedure, or pancreaticoduodenectomy, is a complex operation to remove the head of the pancreas, the first part of the small intestine (duodenum), the gallbladder, and the end of the bile duct, primarily for tumors in that area.
2. Why is it called the Whipple procedure?
It is named after Dr. Allen Whipple, the American surgeon who refined and demonstrated the safety of this complex operation in the 1930s.
3. Is the Whipple procedure a common surgery?
No, it is a highly specialized and relatively uncommon surgery that should only be performed at centers with significant experience.
4. What is the main purpose of the Whipple operation procedure?
Its main purpose is to completely remove tumors in the head of the pancreas, offering the only potential for a cure for pancreatic cancer in that location.
5. Is the Whipple considered a very high-risk surgery?
It is a major surgery with significant risks, but at a high-volume center with an expert surgeon, the mortality risk is low (less than 4%).
6. How long does a Whipple procedure take?
The surgery itself is long and complex, typically lasting between 4 and 8 hours.
7. What does pancreaticoduodenectomy mean?
It literally means the removal (“-ectomy”) of the pancreas (“pancreatico-“) and the duodenum (“-duoden-“).
8. Is the Whipple procedure always for cancer?
Mostly, yes. The vast majority are performed for pancreatic cancer and whipple procedure is the standard. However, it can also be done for other cancers (bile duct, duodenum) or some complex benign conditions.
9. Can the surgery be done laparoscopically or robotically?
Yes, in select patients, a minimally invasive approach can be used. This requires a surgeon with highly advanced skills in these techniques.
10. What is a “pylorus-preserving” Whipple?
This is a variation where the surgeon does not remove the lower part of the stomach and preserves the pylorus (the valve between the stomach and small intestine).
The Surgery Itself: Steps and Anatomy
11. What are the main whipple procedure steps?
The two main phases are resection (removing the organs) and reconstruction (reconnecting the digestive tract).
12. Why do so many organs need to be removed?
Due to the complex whipple procedure anatomy, the head of the pancreas shares blood vessels and tissue planes with the duodenum, bile duct, and gallbladder, so they must be removed together to get the whole tumor out.
13. What happens to the rest of the pancreas?
The remaining body and tail of the pancreas are preserved and reconnected to the small intestine to allow digestive enzymes to flow.
14. How many reconnections does the surgeon make?
The surgeon must skillfully create three new connections (anastomoses): the pancreas to the intestine, the bile duct to the intestine, and the stomach to the intestine.
15. Which part of the reconstruction is the most difficult?
The connection of the soft, delicate pancreas to the intestine is considered the most challenging part and has the highest risk of leaking.
16. Will lymph nodes be removed?
Yes, removing the regional lymph nodes is a critical part of the cancer operation to check for spread and accurately stage the disease.
17. What is the role of the pathologist during the surgery?
A pathologist may examine “frozen sections” of tissue during the operation to help the surgeon ensure they have removed all the cancer (achieving “clear margins”).
18. Will I need a blood transfusion?
This is a long operation and blood loss is a risk. While many patients do not need a transfusion, blood is always available if required.
19. Why is the gallbladder removed?
It is removed because it is attached to the part of the bile duct that must be taken out along with the head of the pancreas.
20. How does the surgeon see what they are doing?
In an open surgery, through a large incision. In a laparoscopic or robotic surgery, using a camera and specialized instruments inserted through small incisions.
Contact & WhatsApp: +90 530 917 30 30
Recovery and Life After Whipple
21. What is the Whipple procedure recovery timeline?
Recovery involves a 1-2 week hospital stay, followed by 2-3 months of recovery at home before energy levels start to normalize.
22. How much pain will I be in after surgery?
Pain is significant but is managed effectively with strong medications, often an epidural or a patient-controlled pump in the first few days.
23. Will I have drains and tubes?
Yes, you will wake up with several temporary drains and tubes (like a nasogastric tube and urinary catheter) which are removed as you recover.
24. When can I eat real food?
You will start with ice chips and liquids, and your diet will be advanced very slowly over several days as your new digestive system “wakes up.”
25. Will I need to take enzyme pills?
Yes, almost all patients need to take prescription pancreatic enzyme pills (PERT) with every meal and snack for the rest of their lives to properly digest food.
26. Will I become diabetic after the Whipple?
It is a risk, as the part of the pancreas that produces insulin is partially removed. Some patients develop diabetes, while others do not.
27. What is the diet like long-term?
The diet focuses on smaller, more frequent meals (5-6 per day) that are high in protein and healthy fats, and low in sugar.
28. Can I live a normal life after a Whipple procedure?
Yes. While there are permanent dietary adjustments, after the recovery period, most patients return to a full and active life.
29. How long will I be off work?
You should plan to be off work for at least 2-3 months.
30. What are the most common long-term side effects?
The most common are digestive changes requiring enzyme pills, and the potential for developing diabetes.
Risks and Survival Rates
31. What is the biggest complication risk of the Whipple procedure?
The most common and serious complication is a pancreatic fistula, which is a leak from the new pancreas-intestine connection.
32. How is a pancreatic fistula treated?
Most leaks are managed non-surgically by leaving drains in place to control the fluid until it heals, but it can prolong the hospital stay.
33. What is the mortality rate for the operation?
At high-volume centers of excellence with expert surgeons, the risk of dying from the surgery itself is low, typically between 2% and 4%.
34. What is the 5-year whipple procedure survival rate for pancreatic cancer?
For patients who have a successful surgery and complete post-operative chemotherapy, the 5-year survival rate is in the range of 20-30%.
35. Does survival depend on the surgeon?
Yes, absolutely. Studies have repeatedly shown that patients have better survival rates when their Whipple is performed by a high-volume, specialist surgeon.
36. What does an “R0 resection” mean and why is it important?
An R0 resection means the surgeon removed all of the tumor with “clean” margins (no cancer cells at the edge). This is the single most important factor for long-term survival.
37. Is the whipple procedure worth it if the cancer might come back?
Yes. It is the only chance to prevent the cancer from coming back. Without the surgery, the cancer will certainly progress.
38. What is delayed gastric emptying?
It’s a common complication where the stomach is slow to empty after surgery, causing nausea and fullness. It is usually temporary and resolves with time.
39. Can you get blood clots?
Yes, this is a risk with any major surgery. You will be given blood thinners to help prevent them.
40. What if my health is not very good? Can I still have a Whipple?
A thorough pre-operative assessment is done to ensure you are strong enough for the surgery. Some health issues may need to be optimized before the operation.
41. Why do I need chemotherapy after surgery?
Chemotherapy is given after surgery (adjuvant therapy) to kill any microscopic cancer cells that may have escaped, reducing the risk of recurrence and improving survival.
42. What happens if the cancer has spread to lymph nodes?
Even if the cancer is in the nearby lymph nodes (which are removed during surgery), the Whipple procedure followed by chemotherapy still offers the best chance for long-term control.
43. Is the survival rate different for other types of cancer (e.g., bile duct)?
Yes, the prognosis for ampullary or bile duct cancer treated with a Whipple is generally better than for pancreatic adenocarcinoma.
44. Does age affect the survival rate?
Age itself is less important than a patient’s overall fitness and other health conditions. Many older patients undergo the surgery successfully.
45. What if the surgeon finds during the operation that the cancer has spread?
In some cases, the surgeon may find small spots of spread (metastases) that were not visible on scans. If this happens, they may stop the Whipple and perform a simpler palliative bypass instead.
46. What is the most hopeful statistic about the Whipple procedure?
The most hopeful fact is that this procedure exists and that it can cure a significant number of patients of a disease that was once considered universally fatal.
47. What if I am too weak for surgery?
Sometimes, pre-operative nutrition support or even a course of chemotherapy can be used to improve a patient’s strength and make them a better candidate for surgery.
48. Does a robotic Whipple have a better survival rate?
Current data suggests that survival rates are equivalent between open and robotic surgery, as long as both are performed by an expert surgeon.
49. Will my life expectancy be normal after a successful Whipple for cancer?
If you are among the fortunate patients who are cured, you can go on to live a normal life expectancy, with adjustments for your new digestive system.
50. How do I maintain hope when reading statistics?
Remember that you are an individual, not a statistic. Your outcome depends on your specific cancer, your body, and the quality of the medical team you choose.
Contact & WhatsApp: +90 530 917 30 30
Choosing a Surgeon and Logistics
51. How do I choose the best surgeon for a Whipple procedure?
Choose a fellowship-trained surgical oncologist or HPB surgeon who performs a high volume of these procedures (at least 15-20 per year) at a major center.
52. Why is a “high-volume” surgeon so important?
Repetition builds mastery. A high-volume surgeon and their team have seen and managed every possible scenario, leading to safer surgery and better results.
53. Is it worth traveling to find the right surgeon?
For a surgery of this magnitude, yes. Traveling for expertise is one of the most important investments you can make in your health.
54. What questions should I ask a potential Whipple surgeon?
Ask “How many of these operations do you do per year?” and “What are your personal complication rates for pancreatic fistula?”.
55. Can I get a second opinion from Prof. Dr. Karatepe?
Yes, we offer remote second opinion services where we can review your scans and medical records to provide our expert assessment.
56. How long would I need to stay in Turkey for the surgery?
You should plan for a total stay of at least 3-4 weeks to account for pre-op testing, the surgery, hospital recovery, and initial post-discharge monitoring.
57. What support is offered for international patients?
We provide comprehensive support, including coordination of travel, accommodation, translation services, and all medical appointments.
58. What is the first step to becoming a patient?
Contact our international patient office. They will guide you on the process of sending your medical information for review.
59. How much does a Whipple procedure cost?
The cost at our center is significantly more affordable than in the US or UK. We provide a transparent, all-inclusive price after reviewing your case.
60. Can a family member stay with me?
Yes, we strongly recommend having a family member or loved one accompany you for support.
Miscellaneous Questions
61. What is the whipple procedure pancreatic cancer connection?
The Whipple is the primary surgical cure for cancers located in the head of the pancreas.
62. Will I have a large scar?
An open Whipple leaves a large scar on the upper abdomen. A minimally invasive approach uses several smaller scars.
63. Can I eat normally after a Whipple?
You will establish a “new normal” of eating smaller, more frequent meals and taking enzyme pills with all food.
64. What do the enzyme pills do?
They replace the digestive enzymes your pancreas used to make, allowing you to break down and absorb fats and proteins.
65. What happens if I forget to take my enzymes?
You will likely experience bloating, gas, and diarrhea (steatorrhea) as your body will be unable to digest the food properly.
66. What is the Whipple’s operation procedure like for the family?
It is a long and stressful day. The surgical team will provide updates during and after the procedure.
67. Will I lose weight after the surgery?
Yes, most patients lose some weight during the recovery period as they adjust to their new digestive system.
68. Can I exercise after I recover?
Yes, returning to regular physical activity is an important part of your long-term health and well-being.
69. Can I drink alcohol?
It is generally recommended to avoid or strictly limit alcohol, as it can be taxing on your remaining pancreas and liver.
70. What are the long-term dietary restrictions?
The main “restriction” is portion size. Many people also find they tolerate high-sugar and very greasy foods poorly.
71. Will I be able to feel the new connections inside me?
No, you will not be able to feel the internal reconnections.
72. How will my bowel movements change?
They may become different in consistency and frequency. Taking your enzymes correctly is the key to maintaining normal bowel function.
73. What is the pancreas?
It’s a gland behind the stomach that makes digestive enzymes and hormones like insulin.
74. Can you live without the head of the pancreas?
Yes. The remaining tail of the pancreas is usually sufficient to produce the insulin the body needs, though this is monitored closely.
75. What is the duodenum?
It is the first part of the small intestine, immediately after the stomach, where much of digestion takes place.
76. Can I get a Whipple if I’ve had previous abdominal surgery?
It is possible but makes the surgery more challenging due to scar tissue. This is another reason why an expert surgeon is essential.
77. What if the surgeon can’t remove the whole tumor?
If the tumor cannot be fully removed, the surgeon may perform a palliative bypass surgery instead to relieve symptoms like jaundice or intestinal blockage.
78. What is a palliative bypass?
It is a simpler operation that reroutes the bile duct and stomach to the intestine to bypass the tumor, relieving blockages but leaving the tumor in place.
79. How do I prepare my home for my return from the hospital?
Have comfortable places to rest, easy-to-prepare soft foods and protein shakes, and a support system in place to help you.
80. Is it normal to feel depressed or anxious after surgery?
Yes, it is very normal. This is a huge physical and emotional event. Seeking support from family, friends, or a professional is important.
81. Will I need follow-up scans?
Yes, you will have regular follow-up CT scans for several years after your surgery to monitor for any signs of recurrence.
82. When can I drive a car?
Not until you are off all narcotic pain medication and can move freely without pain, usually at least 4-6 weeks after surgery.
83. What is the most challenging part of recovery?
For many, it’s regaining their strength and appetite and adjusting to the new way of eating.
84. Can I travel on an airplane after I recover?
Yes, once you are fully recovered, you can travel freely.
85. Will I need a special diet forever?
You will need a mindful approach to eating for the rest of your life, focusing on small, nutrient-dense meals.
86. What is a Whipple procedure pancreatic indication other than cancer?
Severe, painful chronic pancreatitis with an enlarged head of the pancreas, or a large benign tumor causing symptoms.
87. What does the “head” of the pancreas do?
It is where the main pancreatic duct joins the bile duct to empty into the duodenum. It is a critical crossroads for digestion.
88. How important is a positive attitude?
While not a substitute for expert medical care, a determined and positive mindset can be a powerful asset during the challenging recovery period.
89. What is the first thing I can drink after surgery?
You will start with sips of water or ice chips, and slowly progress to other clear liquids.
90. Will I be in the ICU (Intensive Care Unit)?
Most patients spend the first night or two in an ICU or a high-dependency step-down unit for close monitoring.
91. Can you explain the whipple procedure anatomy in a simple way?
Imagine the head of the pancreas is a central railway station. A tumor there blocks all the tracks. The Whipple removes the station and then rebuilds the tracks (intestine, bile duct, pancreas) to create a new, functional junction.
92. Is the whipple operation procedure always the same?
The core principles are the same, but the surgeon may make slight technical modifications based on a patient’s individual anatomy.
93. What if I am told I’m not a candidate for a Whipple?
It is always worthwhile to get a second opinion from a high-volume Whipple surgeon, as they may be able to operate on cases that others deem unresectable.
94. How many Whipple procedures has Prof. Dr. Karatepe performed?
He has performed hundreds of major pancreatic and abdominal cancer operations over his 25+ year career, making him a true master of the procedure.
95. What is the biggest myth about the Whipple procedure?
Perhaps the biggest myth is that it’s not survivable. With modern techniques and expert surgeons, it is a safe operation that saves lives.
96. Will I be able to taste and enjoy food again?
Yes, absolutely. After you recover, you will be able to enjoy a wide variety of healthy foods.
97. What is the most important advice for a patient?
Choose your surgeon wisely. Your choice of surgeon is the most important decision you will make.
98. Will my family get support too?
Yes, we understand this is a journey for the whole family, and our team is here to support them with information and guidance.
99. How soon can I get a consultation?
We prioritize urgent cases like this. Contact our team, and we will arrange a consultation as quickly as possible.
100. I’m ready to fight. What is my first step?
Your first step is to arm yourself with the best expert you can find. Contact us to start the process of getting a world-class opinion on your case.
Contact & WhatsApp: +90 530 917 30 30
References
We base our practice and information on the highest standards set by leading global medical authorities and cancer research organizations. The content on this page is informed by:
- Johns Hopkins Medicine, The Sol Goldman Pancreatic Cancer Research Center. (n.d.). The Whipple Procedure. https://pathology.jhu.edu/pancreas/treatment-surgery/whipple-procedure
- Mayo Clinic. (n.d.). Whipple procedure. https://www.mayoclinic.org/tests-procedures/whipple-procedure/about/pac-20385074
- Pancreatic Cancer Action Network (PanCAN). (n.d.). Whipple Procedure (Pancreaticoduodenectomy). https://pancan.org/facing-pancreatic-cancer/treatment/treatment-types/surgery/whipple-procedure-pancreaticoduodenectomy/
Please note: This information is for general purposes only. For personalized treatment advice, please contact us directly.
